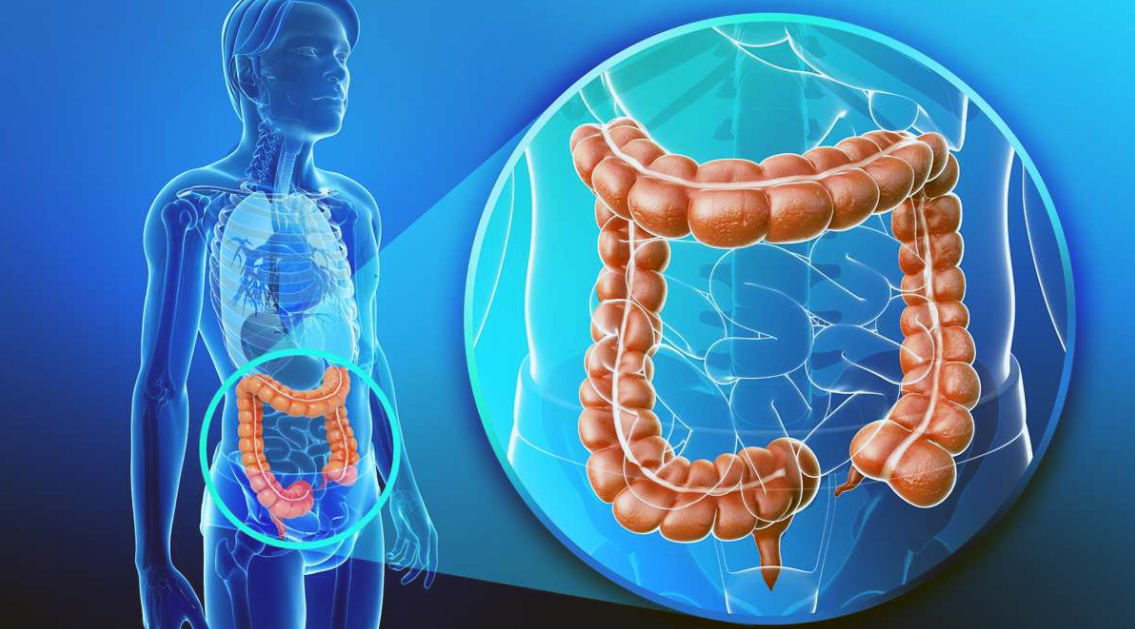
Similar to Chron’s disease, Ulcerative colitis is a chronic inflammatory disease affecting large intestine’s mucosa. There’s recurring inflammation going on in a superficial layer of the intestinal wall leading to lesions, abnormal digestion and a wide range of tough symptoms. Many theories suggest various explanations, but none has a definite answer to what causes ulcerative colitis. The most probable explanation is an excessive immune reaction where immune cells attack food and bacteria normally situated in the large intestine. The lining becomes damaged, scattered with ulcers and dysfunctional. That creates clinical picture consisting of diarrhea, often followed by rectal bleeding, abdominal pain, fatigue, fever, weight, and appetite loss. The severity of symptoms varies, but their presence always affects the quality of everyday’s life. Since millions of people around the world suffer from ulcerative colitis and every patient is at high risk of getting colon cancer, this condition draws the attention of the medical community and various scientists.
Is symptomatic therapy the best we got so far?
 Unfortunately, when the main cause is unknown, the only way to treat the condition is to decrease its risk factors and suppress its symptoms. The current official approach involves immune system suppressors, anti – inflammatory medications, antibiotics, anti – diarrheal drugs, painkillers, and various supplements to compensate substances lost due to diarrhea. Patients with complications or severe symptoms resistant to medications can be treated surgically, but this usually means surgical removal of a big portion or entire large intestine. Recently, some new ideas and promising therapy strategies are being explored and tested.
Unfortunately, when the main cause is unknown, the only way to treat the condition is to decrease its risk factors and suppress its symptoms. The current official approach involves immune system suppressors, anti – inflammatory medications, antibiotics, anti – diarrheal drugs, painkillers, and various supplements to compensate substances lost due to diarrhea. Patients with complications or severe symptoms resistant to medications can be treated surgically, but this usually means surgical removal of a big portion or entire large intestine. Recently, some new ideas and promising therapy strategies are being explored and tested.
Fecal microbiota transplantation brings hope to UC patients
 This relatively new procedure, also known as stool transplantation, has been used to cure colitis caused by bacteria Clostridium difficult. Since many studies have shown the important role of intestine bacteria in the genesis of ulcerative colitis, recent trials are trying to apply fecal microbiota transplants as a treating method for UC patients. The major idea is to collect stool samples from healthy donors, prepared them in a special way and place into colon tissue of people suffering from UC. The transplantation is conducted via colonoscopy, endoscopy or enema. Donor’s stool contains good and useful intestinal bacteria needed for normal physiology of the bowls and allegedly being killed by immune cells in ulcerative colitis, causing predomination of pathogenic bacteria in bowls.
This relatively new procedure, also known as stool transplantation, has been used to cure colitis caused by bacteria Clostridium difficult. Since many studies have shown the important role of intestine bacteria in the genesis of ulcerative colitis, recent trials are trying to apply fecal microbiota transplants as a treating method for UC patients. The major idea is to collect stool samples from healthy donors, prepared them in a special way and place into colon tissue of people suffering from UC. The transplantation is conducted via colonoscopy, endoscopy or enema. Donor’s stool contains good and useful intestinal bacteria needed for normal physiology of the bowls and allegedly being killed by immune cells in ulcerative colitis, causing predomination of pathogenic bacteria in bowls.
Promising results of the first multicentric FMT study
 During Digestive Disease Week 2016 in San Diego, a team of scientists from University of New South Wales presented the results of their recent research regarding usage of FMT in treatment patients with ulcerative colitis. The study involved 81 patient divided into two groups. The first group, randomly chosen, received FMT treatment and others received placebo. This was the first trial to use intense therapy of 40 FMT infusions over eight weeks and involve a significant number of participants. Researchers monitored the evolution of symptoms and examined the intestinal mucosa endoscopically during the trial and came up with the quite promising conclusion. 27 percent of patients who received FMT reported weakened or completely gone symptoms followed by endoscopic signs of healing colon lining. Only 8 percent of participants receiving placebo showed improvement in these two ways.
During Digestive Disease Week 2016 in San Diego, a team of scientists from University of New South Wales presented the results of their recent research regarding usage of FMT in treatment patients with ulcerative colitis. The study involved 81 patient divided into two groups. The first group, randomly chosen, received FMT treatment and others received placebo. This was the first trial to use intense therapy of 40 FMT infusions over eight weeks and involve a significant number of participants. Researchers monitored the evolution of symptoms and examined the intestinal mucosa endoscopically during the trial and came up with the quite promising conclusion. 27 percent of patients who received FMT reported weakened or completely gone symptoms followed by endoscopic signs of healing colon lining. Only 8 percent of participants receiving placebo showed improvement in these two ways.
The brighter future?
Many new questions popped up after this study and many experts are concerned about long – term effects of this therapy, but the research has shown beyond any doubt that fecal microbiota transplantation could be used in the future as an effective treatment for patients with ulcerative colitis. According to some scientists, the treatment should have positive results – at least 60% of cases should have the positive outcome.